The 26 bones and 30 joints1Manganaro D, Dollinger B, Nezwek TA, Sadiq NM. Anatomy, Bony Pelvis and Lower Limb, Foot Joints. In: StatPearls. StatPearls Publishing; 2023. Accessed November 14, 2023. http://www.ncbi.nlm.nih.gov/books/NBK536941/ in the foot and ankle are at risk for running injuries. Many of these injuries that occur secondary to regular running or jogging, such as Achilles tendonitis and heel bursitis, begin with mild pain that gets worse over time.
To stop foot or ankle pain from getting worse, a runner must first understand their condition and recognize its symptoms—what it feels like.
The following are common foot and ankle injuries in runners, including their descriptions and classic symptoms:
In This Article:
- Common Running Injuries: Knee Pain
- Common Running Injuries: Foot and Ankle Pain
- Common Running Injuries: Calf and Shin Pain
- Common Running Injuries: Hip or Thigh Pain
- Common Running Injuries: Back Pain
Plantar Fasciitis2Trojian T, Tucker AK. Plantar Fasciitis. afp. 2019;99(12):744-750. Accessed November 5, 2023. https://www.aafp.org/pubs/afp/issues/2019/0615/p744.html
Plantar fasciitis is inflammation of the plantar fascia, causing stabbing heel pain.
Affecting runners and nonrunners alike, plantar fasciitis causes painful symptoms ranging from annoying to debilitating. This condition is also called plantar fasciopathy.
What it is: The plantar fascia is a thick band of fibrous tissue that runs between the toes and heel. It stretches and contracts thousands of times daily with each step or stride. If the area where the plantar fascia attaches to the heel bone becomes damaged, it is called plantar fasciitis.
How it feels: Plantar fasciitis tends to cause stabbing heel pain that is worse in the morning, especially during the first few steps out of bed, and at the end of the day. Pressing on the inside (medial side) of the heel may feel painful, like a bruise. See Plantar Fasciitis Symptoms
Nonsurgical treatments, such as stretching the plantar fascia, work in 8 out of 10 cases. See Plantar Fasciitis: Initial Treatment Options
Read more about Plantar Fasciitis
Achilles Tendinopathy (Tendinitis)3Silbernagel KG, Hanlon S, Sprague A. Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. J Athl Train. 2020;55(5):438-447. doi:10.4085/1062-6050-356-19
Achilles tendon inflammation causes pain above the back of the heel.
Though it can affect athletes and non-athletes alike, Achilles tendinopathy is most common in runners and other athletes who ramp up their training too quickly.
What it is: The Achilles tendon connects the gastrocnemius and soleus muscles in the calf to the back of the heel. If the tendon tissue breaks down or fails to heal from a tear, it is called tendinopathy.
While the term Achilles tendonitis is popular, doctors prefer to use the term Achilles tendinopathy. Tendonitis requires the tendon to be inflamed, and not all chronic Achilles pain involves inflammation.
How it feels: Pain is typically felt above the back of the heel and affects a person’s ability to run as fast and comfortably as normal. Stiffness, swelling, and tenderness may also be noticeable. Symptoms may be worse first thing in the morning or after a workout. See Achilles Tendon Conditions Signs and Symptoms
Blood flow to the area above the back of the heel is limited, so healing tends to be slow. Treatment requires patience. See Treating a Painful Achilles Tendon
Read more about Achilles Tendonitis and Tendon Injuries
Ankle Sprain
Ankle sprain occurs when the ligaments in the ankle joint are over-stretched or torn.
A runner may sprain an ankle if a foot twists inward or outward when it hits the ground —what many people call rolling an ankle.
What it is: An ankle sprain is not an overuse injury but a one-time traumatic injury. It occurs when a ligament that connects two bones in the ankle joint is overstretched, partially torn, or completely torn.
How it feels: The pain of a sprain is immediate and usually accompanied by ankle swelling. The person may not be able to put weight on the affected foot. See Ankle Sprain and Strain Signs and Symptoms
Like many other acute injuries, an ankle sprain can be first treated with R.I.C.E: Rest, Ice, Compression, and Elevation. See Ankle Sprain and Strain Treatment Options
Read more about Ankle Sprains and Strains
Stress Fracture in the Foot or Ankle4Vera AM, Patel KA. Stress Fractures of the Foot and Ankle. Operative Techniques in Sports Medicine. 2021;29(3):150852. doi:10.1016/j.otsm.2021.150852
Foot stress fracture commonly affects bones such as the metatarsals, navicular, and calcaneus bone.
Almost all stress fractures in the foot and ankle occur in runners and other athletes. The bones most likely to be broken include:
- Metatarsals, the long bones that join with the toes
- Navicular bone, a concave bone at the top and back of the foot
- Calcaneus, or heel bone—particularly the back of the heel bone
People diagnosed with osteoporosis or osteopenia have less dense bones and are more likely to get this condition.
What it is: A stress fracture is a broken bone. A crack in the bone develops gradually through repetitive pressure. Stress fractures in the foot or ankle are often associated with intense running schedules and not enough recovery time.
How it feels: The pain of a stress fracture in the foot or ankle sneaks up over time. Pain is worse when running, walking, or standing and less noticeable when sitting or lying down. See Symptoms of a Foot Stress Fracture
Pressing down on the skin over the affected bone may cause a lot of pain. As the pain gets worse, the foot may appear swollen and bruised.
Stress fractures can be difficult to see on a standard X-ray. A definitive diagnosis may require an MRI or bone scan, though this step is not always necessary before nonsurgical treatment. Recovery takes several weeks. See Foot Stress Fracture: Treatment Options, Recovery, and Prevention
Read more about Foot Stress Fractures
Metatarsalgia
Too much pressure on the long metatarsal bones in the foot can lead to a painful condition called metatarsalgia. Intense running training, poorly fitting footwear, and high arches are often linked to this condition.5Besse JL. Metatarsalgia. Orthop Traumatol Surg Res. 2017;103(1S):S29-S39. doi:10.1016/j.otsr.2016.06.020
What it is: Metatarsalgia is defined as pain in the front part of the foot, where the long metatarsal bones in the foot end. Nine out of 10 cases of metatarsalgia are related to problems with biomechanics5Besse JL. Metatarsalgia. Orthop Traumatol Surg Res. 2017;103(1S):S29-S39. doi:10.1016/j.otsr.2016.06.020—the foot’s anatomy and how it moves during walking and running.
How it feels: Pain is felt right behind the base of the toes, often in the ball of the foot. Exactly where the pain appears and how it feels will depend on the cause. For example, a rare condition called Frieberg’s disease is most likely to cause pain behind the second or third toe.5Besse JL. Metatarsalgia. Orthop Traumatol Surg Res. 2017;103(1S):S29-S39. doi:10.1016/j.otsr.2016.06.020,6Carter KR, Chambers AR, Dreyer MA. Freiberg Infraction. In: StatPearls. StatPearls Publishing; 2023. Accessed November 10, 2023. http://www.ncbi.nlm.nih.gov/books/NBK537308/
Metatarsalgia is most notable when running, walking, or standing. Some people with metatarsalgia are later diagnosed with osteoarthritis, the most common type of arthritis.
Morton’s Neuroma
Doctors may call this painful foot condition interdigital neuroma, Morton metatarsalgia, interdigital neuritis, or plantar neuroma. It is common in runners because each time a foot pushes off the ground, the joints in the ball of the foot hyperextend under pressure.
What it is: A group of nerves, called plantar nerves, branch out along the bottom of the foot to the toes. Repeated pressure and hyperextension of the joints in the ball of the foot causes unwanted tissue to grow in and around a nerve. When tissue squeezes or compresses a nerve, it’s called Morton’s neuroma.
How it feels: Morton’s neuroma causes foot pain that feels like cramping, burning, tingling, or numbness. Runners sometimes often say they feel like a lump or pebble is stuck in a shoe. Symptoms are most likely to occur between the base of the third and fourth toes or the second and third toes.7Carroll LA, Paulseth S, Martin RL. Forefoot Injuries in Athletes: Integration of the Movement System. Int J Sports Phys Ther. 17(1):81-89. doi: 10.26603/001c.30021
It’s best to treat Morton’s neuroma early, before it gets worse or becomes chronic.
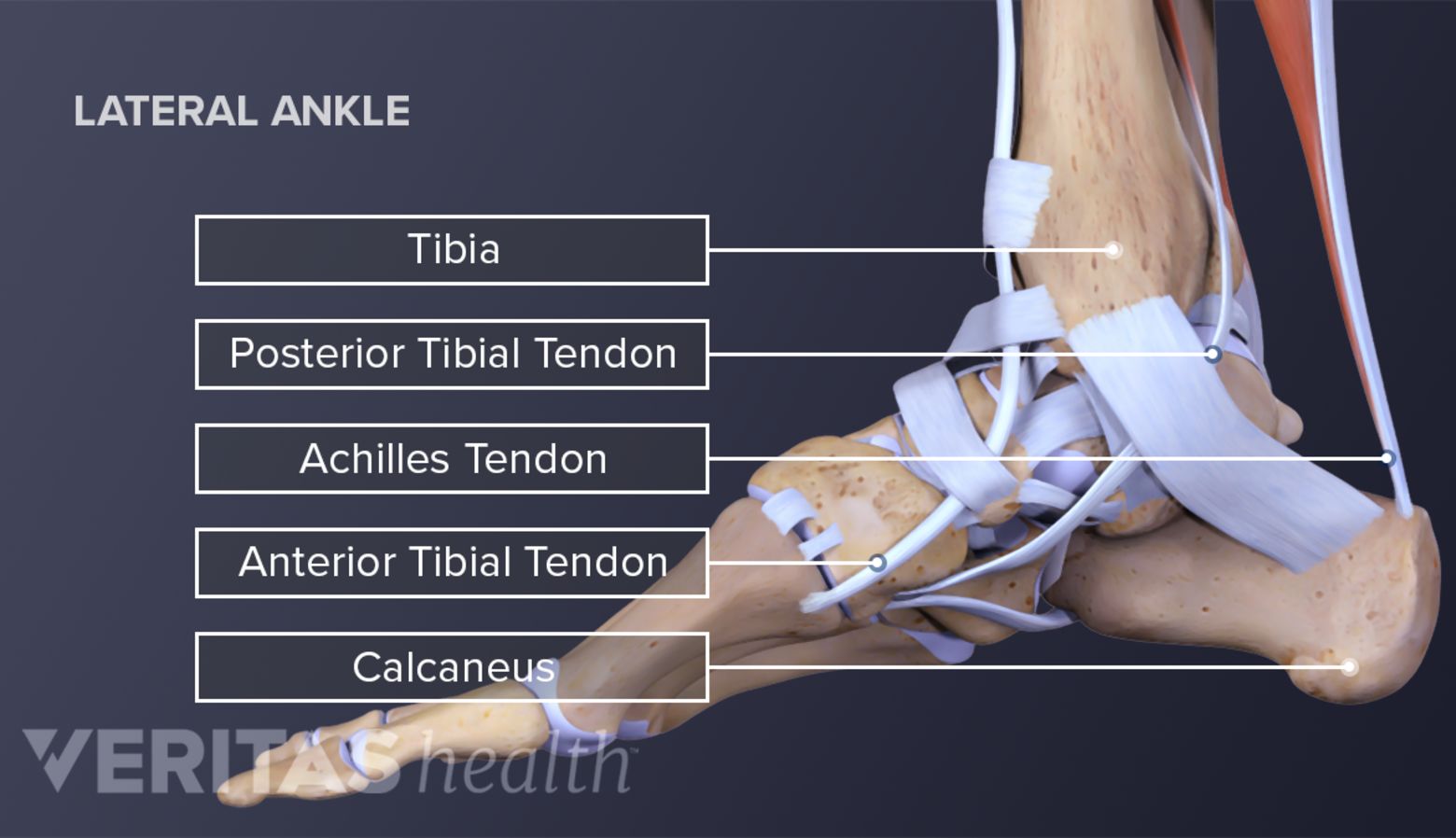
Posterior Tibial Tendon Dysfunction8Park S, Lee J, Cho HR, Kim K, Bang YS, Kim YU. The predictive role of the posterior tibial tendon cross-sectional area in early diagnosing posterior tibial tendon dysfunction. Medicine (Baltimore). 2020;99(36):e21823. doi:10.1097/MD.0000000000021823
Dysfunction of the posterior tibial tendon occurs when it becomes inflamed or torn from overuse.
Usually linked to flat feet, posterior tibial tendon dysfunction typically develops over time in runners and other athletes. This condition may also be called posterior tibial tendinitis.
What it is: Deep in the calf is a muscle called the tibialis posterior muscle, or posterior tibial muscle. This muscle is connected to the foot by a tendon. If that tendon becomes inflamed or torn from overuse, it is called posterior tibial tendinitis or dysfunction.
How it feels: Runners and other athletes with posterior tibial tendon dysfunction may notice the affected foot’s arch getting flatter over time. As the foot flattens, the ankle may begin to collapse inward.
This condition tends to cause pain in the ankle or the area where the ankle meets the foot. This pain gets worse with running or other activities. Swelling, warmth, and redness are often seen if inflammation is present (tendonitis).
Runner’s Toe (Black Toenails)
The medical name for this blackened toenails is subungual hematoma.9Lee DK, Lipner SR. Optimal diagnosis and management of common nail disorders. Annals of Medicine. 2022;54(1):694-712. doi:10.1080/07853890.2022.2044511 Runners tend to develop this condition if their toes repeatedly jam into the front of their shoes. This toe jamming can occur while running downhill or in shoes that are too small or too big.
What it is: Repeated mini-traumas to the toes can cause blood to collect, much like when a bruise develops. The blood becomes trapped under the nail.
How it feels: The most obvious symptom of this condition is not how it feels but how it looks—the toenail bed will appear black, brown, purple, or dark red3Silbernagel KG, Hanlon S, Sprague A. Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. J Athl Train. 2020;55(5):438-447. doi:10.4085/1062-6050-356-19. Pain is also possible, especially if the toe area is squeezed. The nail may get thick, crack, split, or come off.
Blisters
While rarely serious, blisters are painful. Distance runners often get blisters on their toes, ball of the foot, heel, or sole.10Scheer BV, Reljic D, Murray A, Costa RJS. The Enemy of the Feet: Blisters in Ultraendurance Runners. Journal of the American Podiatric Medical Association. 2014;104(5):473-478. doi:10.7547/0003-0538-104.5.473
What it is: A blister is a bubble of fluid trapped under a layer of skin. In runners, blisters usually develop in areas where a foot rubs uncomfortably against a shoe. This friction causes layers of the skin to split and separate, and fluid collects in the space.10Scheer BV, Reljic D, Murray A, Costa RJS. The Enemy of the Feet: Blisters in Ultraendurance Runners. Journal of the American Podiatric Medical Association. 2014;104(5):473-478. doi:10.7547/0003-0538-104.5.473
How it feels: Even a small blister causes pain with every step. Experienced distance runners have dropped out of races due to severe blister pain.10Scheer BV, Reljic D, Murray A, Costa RJS. The Enemy of the Feet: Blisters in Ultraendurance Runners. Journal of the American Podiatric Medical Association. 2014;104(5):473-478. doi:10.7547/0003-0538-104.5.473
Heel (Retrocalcaneal) Bursitis
Retrocalcaneal bursitis causes pain, tenderness, and swelling at the back of the heel.
Running, particularly running uphill, causes the foot to flex considerably. This flexion can be especially irritating to a retrocalcaneal bursa.
What it is: The retrocalcaneal bursa is a small, fluid-filled sac located between the heel bone and the Achilles tendon. Normally, this bursa works as a cushion and lubricant between the two structures. If repeated foot flexion causes the bursa to become irritated and inflamed, it is called retrocalcaneal bursitis.
How it feels: Retrocalcaneal bursitis causes pain, tenderness, and swelling at the back of the heel.
Because the symptoms are similar, heel bursitis and Achilles tendonitis are often mistaken for one another. Moreover, a person can have both conditions at the same time. For example, if Achilles tendonitis is left untreated, it might lead to retrocalcaneal bursitis.
See Heel (Retrocalcaneal and Calcaneal) Bursitis on Arthritis-health.com
As with most injuries, these foot and ankle conditions are easier to treat in the early stages. It’s a good idea to get medical attention if the pain in the foot or ankle does not resolve after 2 or 3 weeks of rest or if the pain is severe.
Runners are advised to make an appointment with a physiatrist, podiatrist, orthopedist, or primary care physician for a diagnosis and treatment plan.
- 1 Manganaro D, Dollinger B, Nezwek TA, Sadiq NM. Anatomy, Bony Pelvis and Lower Limb, Foot Joints. In: StatPearls. StatPearls Publishing; 2023. Accessed November 14, 2023. http://www.ncbi.nlm.nih.gov/books/NBK536941/
- 2 Trojian T, Tucker AK. Plantar Fasciitis. afp. 2019;99(12):744-750. Accessed November 5, 2023. https://www.aafp.org/pubs/afp/issues/2019/0615/p744.html
- 3 Silbernagel KG, Hanlon S, Sprague A. Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. J Athl Train. 2020;55(5):438-447. doi:10.4085/1062-6050-356-19
- 4 Vera AM, Patel KA. Stress Fractures of the Foot and Ankle. Operative Techniques in Sports Medicine. 2021;29(3):150852. doi:10.1016/j.otsm.2021.150852
- 5 Besse JL. Metatarsalgia. Orthop Traumatol Surg Res. 2017;103(1S):S29-S39. doi:10.1016/j.otsr.2016.06.020
- 6 Carter KR, Chambers AR, Dreyer MA. Freiberg Infraction. In: StatPearls. StatPearls Publishing; 2023. Accessed November 10, 2023. http://www.ncbi.nlm.nih.gov/books/NBK537308/
- 7 Carroll LA, Paulseth S, Martin RL. Forefoot Injuries in Athletes: Integration of the Movement System. Int J Sports Phys Ther. 17(1):81-89. doi: 10.26603/001c.30021
- 8 Park S, Lee J, Cho HR, Kim K, Bang YS, Kim YU. The predictive role of the posterior tibial tendon cross-sectional area in early diagnosing posterior tibial tendon dysfunction. Medicine (Baltimore). 2020;99(36):e21823. doi:10.1097/MD.0000000000021823
- 9 Lee DK, Lipner SR. Optimal diagnosis and management of common nail disorders. Annals of Medicine. 2022;54(1):694-712. doi:10.1080/07853890.2022.2044511
- 10 Scheer BV, Reljic D, Murray A, Costa RJS. The Enemy of the Feet: Blisters in Ultraendurance Runners. Journal of the American Podiatric Medical Association. 2014;104(5):473-478. doi:10.7547/0003-0538-104.5.473