Non-surgical treatments are generally successful in treating non-displaced or minimally displaced proximal humerus fractures where the bones remain in their normal anatomical positions.
Surgery may be necessary when bones are severely displaced and cannot be rejoined without more invasive treatment.
In This Article:
- Proximal Humerus Fractures of the Shoulder
- Treating a Proximal Humerus Fracture
Non-Surgical Treatment for Proximal Humerus Fracture
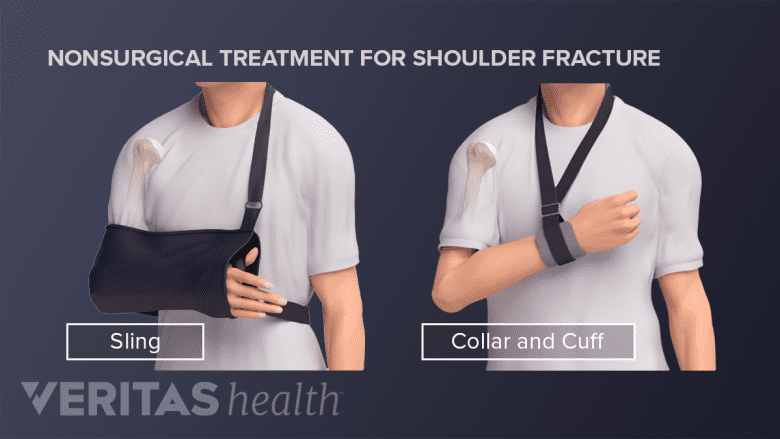
A sling provides support and stability to a healing shoulder and comes in various types and shapes.
Most cases of proximal humerus fractures are treated with non-surgical methods, which include some combination of:
- Medication: Over-the-counter or prescription pain-relieving medication help reduce pain and include:
- Acetaminophen (Tylenol): for mild pain
- Codeine and acetaminophen (Tylenol with Codeine): for mild to moderate pain
- Propoxyphene and acetaminophen (Darvocet N-100, Propacet): for mild to moderate pain
- Hydrocodone and acetaminophen (Lortab, Norcet, Vicodin): for moderate to severe pain
NSAIDs are typically avoided because they reduce inflammation, which can delay or inhibit bone healing and fusion.
- Immobilization: Wearing a sling immobilizes the joint, provides arm support, and protects the injured arm and shoulder. Some people prefer a swathe that wraps horizontally around the chest and arm and further reduces movement, providing extra support and protection.
- Immobilization is recommended for about 2 to 3 weeks, but the exact amount of time varies on the fracture type, age of the patient, and co-occurring medical conditions.
- Physical therapy: Gentle therapeutic exercises, such as pendulum swings, are recommended around 10 to 14 days following the injury. Physical therapy continues for several weeks after the bone has healed to strengthen the shoulder muscles and reduce the risk of future injury.
Non-surgical treatments often have high success rates, with approximately 80% to 85% of patients experiencing a full recovery.1Pencle F, Varacallo M. Proximal Humerus Fracture. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470346/
Potential Complications of Non-Surgical Treatment
In rare cases, non-surgical treatments of proximal humerus fractures can result in long-term complications, including:
- Shoulder stiffness
- Posttraumatic arthritis of the joint
- Poor function of the shoulder
- Bone death caused by an insufficient blood supply (avascular necrosis)
In some cases, if the fractured upper arm bone is immobilized for too long, the patient may be unable to move the shoulder (a condition called frozen shoulder or adhesive capsulitis).
Surgery for Proximal Humerus Fracture
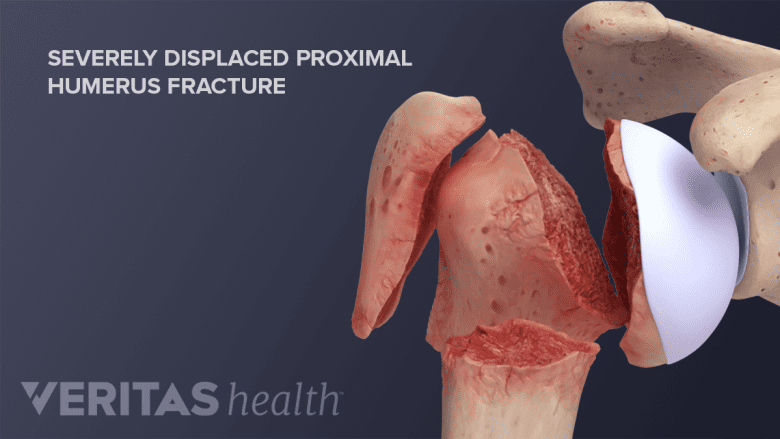
Certain types of severe fractures require surgical treatment to align the bone fragments back in place.
Surgery is considered in cases where there is a high risk of complications or when the displaced bone cannot heal with non-surgical treatments. These situations include:
- Severe displacement: When the bone fragments are significantly out of place
- Dislocated fractures: The humeral head has dislocated from the shoulder socket
- Open fractures: The broken bone penetrates the skin
- Head splitting: If the head (ball) of the humerus is fractured into multiple pieces
- Neurovascular compromise: If the nerves or blood vessels around the shoulder are damaged or at risk
- Failed non-surgical treatment: If immobilization and physical therapy are unsuccessful in relieving pain or improving function
Surgical intervention is more common in younger patients than in older individuals.
Types of Surgery
Both variations of shoulder replacement surgery are used to treat complex proximal humeral fractures.
Surgical options for proximal humerus fracture include:
- Closed reduction and percutaneous pinning (CRPP): manipulating the bone fragments back into place without open surgery and securing them with pins inserted through the skin. This procedure is generally used for minimally displaced fractures with good bone quality.
- Open reduction and internal fixation (ORIF): making an incision to expose the fracture site, realigning the bone fragments, and securing them with implants, such as plates, screws, or wires. This procedure is used for more complex fractures.
- Hemiarthroplasty: replacing the damaged ball part of the shoulder joint with a prosthetic implant. This surgery is reserved for patients with severe fractures and osteoporosis.
- Total shoulder arthroplasty: replacing both the ball and socket of the shoulder joint. This procedure is recommended for complex fractures or when arthritis is present.
- Reverse total shoulder arthroplasty (reverse TSA): a surgical procedure used to treat complex proximal humerus fractures, particularly in older patients with significant bone loss or rotator cuff tears. Unlike a traditional shoulder replacement, the ball and socket are both replaced but in “reverse” alignment from normal anatomy.
Surgical success varies widely and depends on factors such as the severity of the fracture, the patient's age and overall health, the type of surgery, and the surgeon’s skill.
Potential Complications of Surgery
As with any surgical procedure, there are potential risks and complications involved, such as infection, severe bleeding, and nerve or blood vessel damage.
In particular, surgical fixation of the proximal humerus in elderly patients carries a high risk of implant failure and reoperation. People who undergo these surgeries also face similar risks as people who undergo non-surgical treatment, such as shoulder arthritis.
Post-Surgical Rehabilitation
The physician provides specific post-surgery instructions to fit the patient’s individual needs and goals. General guidelines include:
- Wearing a sling for 3 or 4 weeks after surgery.
- Icing the shoulder for 15 to 20 minutes several times a day to reduce swelling.
Wrap the ice pack in a towel or cloth to prevent ice burn and wait for at least 2 hours before re-applying the pack. - Restraining from lifting objects weighing over five pounds during the first six weeks post-surgery.
- Following up with the physician and getting the appropriate x-rays to confirm healing.
- Participating in physical therapy and exercises as formulated by the therapist.
Healing is generally slower in people who have diabetes or who use nicotine-based products (smoking, vaping, or chewing tobacco) since nicotine inhibits bone healing.
- 1 Pencle F, Varacallo M. Proximal Humerus Fracture. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470346/