There are both nonsurgical and surgical treatment options for posterior cruciate ligament (PCL) knee injuries. Surgery is typically only recommended for the most severe tears and for people who have multiple ligament injuries.
In This Article:
- Posterior Cruciate Ligament (PCL) Injuries
- Symptoms of Posterior Cruciate Ligament (PCL) Tears
- Posterior Cruciate Ligament (PCL) Tears: Causes and Risk Factors
- Diagnosing Posterior Cruciate Ligament (PCL) Tears
- Posterior Cruciate Ligament (PCL) Tear Treatment Options
Nonsurgical Treatment Options for PCL Injuries
Less severe posterior cruciate ligament (PCL) tears of the knee generally heal well without surgery. Immediately after the injury, management consists of the RICE method:
- Rest. Any activities that causes knee pain, such as running or walking, should be avoided until symptoms are relieved.
- Ice. A person may be advised to apply ice to the area to help reduce pain and swelling. Ice can be applied several times throughout the day for about 10 to 20 minutes at a time.
- Compression. Swelling can be managed by wearing an elastic bandage around the affected knee.
- Elevation. Keeping the knee supported above the waist can help with swelling.
See The P.R.I.C.E. Protocol Principles
In addition to the RICE method, there are other nonsurgical treatment options available.
- Take non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs, such as ibuprofen (Advil) or naproxen (Aleve) can help relieve pain and swelling.
- Wear a knee brace. A knee brace provides stability and restricts side-to-side movement. Some people may choose to wear a functional knee brace, which allows for more movement, when they return to activity.
- Use crutches. Crutches may be recommended to keep weight off the injured knee.
- Work with a physical therapist. A physical therapist will focus on improving mobility, strength, flexibility, and balance, which can help speed up recovery time and improve performance once the injury has healed.
Recovery time using nonsurgical treatment will vary from person to person and can take anywhere from a few weeks to a few months. Surgery may be recommended in some cases, particularly cases involving severe PCL tears, multiple ligament injuries, or chronic knee instability.
Regenerative Medicine
Regenerative medicine, such as platelet-rich plasma (PRP) treatment, may be recommended to certain people with PCL tears. PRP may be injected or applied during surgery, however there has been little clinical research on the effectiveness of these treatments.
Surgery for PCL Tears
Surgical treatment for posterior cruciate ligament tears remains controversial in the medical community.1Lee BK, Nam SW. Rupture of posterior cruciate ligament: diagnosis and treatment principles. Knee Surg Relat Res. 2011;23(3):135–141. doi:10.5792/ksrr.2011.23.3.135 Kim YM, Lee CA, Matava MJ. Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2011 Feb;39(2):425-34. doi: 10.1177/0363546510374452. Epub 2010 Aug 11. Review. PubMed PMID: 20702860. Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995 Oct;11(5):526-9. PubMed PMID: 8534292. Bergfeld JA, Graham SM, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstructions using single- and double-bundle tibial inlay techniques. Am J Sports Med. 2005;33(7):976-981. Shelbourne KD, Benner RW, Ringenberg JD, Gray T. Optimal management of posterior cruciate ligament injuries: current perspectives. Orthop Res Rev. 2017;9:13–22. Published 2017 Apr 5 Generally, surgery is only recommended for those who have grade III PCL tears, multiple ligament injuries (such as a PCL and ACL tear), and knee instability that has not responded to nonsurgical treatment.
PCL Reconstruction Surgery
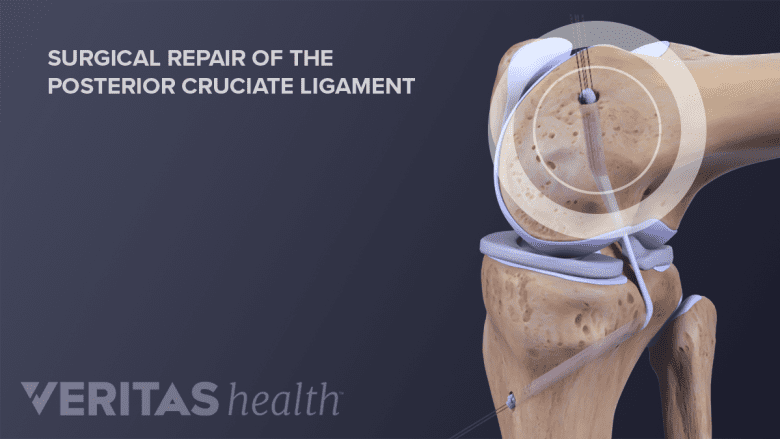
Surgical repair of the PCL is minimally invasive and utilizes graft tissue to reconstruct the ligament.
PCL surgery involves using a graft to reconstruct the ligament. The graft can either be an autograft or allograft.
- Autograft. A piece of tissue from elsewhere on the person’s body, such as the patellar tendon.
- Allograft. A piece of tissue from a donor or cadaver.
This surgery uses an arthroscopic approach, which is a minimally invasive technique that uses special surgical tools and a video camera inserted through small incisions in the knee joint. Special surgical devices, such as screws, anchors, or buttons, secure one end of the graft to the femur (thigh bone) and the other end to the tibia (shin bone).
PCL Surgery Recovery
Recovering from PCL surgery typically does not require an overnight stay in the hospital. Most people will use crutches for the first few days after surgery and some may wear a restrictive brace that prevents the knee from bending.
A formal physical therapy or rehabilitation program is typically started 1 to 4 weeks following surgery. Physical therapy generally consists of stretches and exercises in order to:
- Increase strength
- Improve and restore balance
- Improve range of motion
A full recovery from PCL reconstruction can take anywhere between 9 months and a year, depending on the severity of the tear and if there were any other ligament injuries. Most people should be able to return to pre-injury activities. Some people may need to switch to low impact exercises, such as swimming or biking.
- 1 Lee BK, Nam SW. Rupture of posterior cruciate ligament: diagnosis and treatment principles. Knee Surg Relat Res. 2011;23(3):135–141. doi:10.5792/ksrr.2011.23.3.135 Kim YM, Lee CA, Matava MJ. Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2011 Feb;39(2):425-34. doi: 10.1177/0363546510374452. Epub 2010 Aug 11. Review. PubMed PMID: 20702860. Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995 Oct;11(5):526-9. PubMed PMID: 8534292. Bergfeld JA, Graham SM, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstructions using single- and double-bundle tibial inlay techniques. Am J Sports Med. 2005;33(7):976-981. Shelbourne KD, Benner RW, Ringenberg JD, Gray T. Optimal management of posterior cruciate ligament injuries: current perspectives. Orthop Res Rev. 2017;9:13–22. Published 2017 Apr 5


